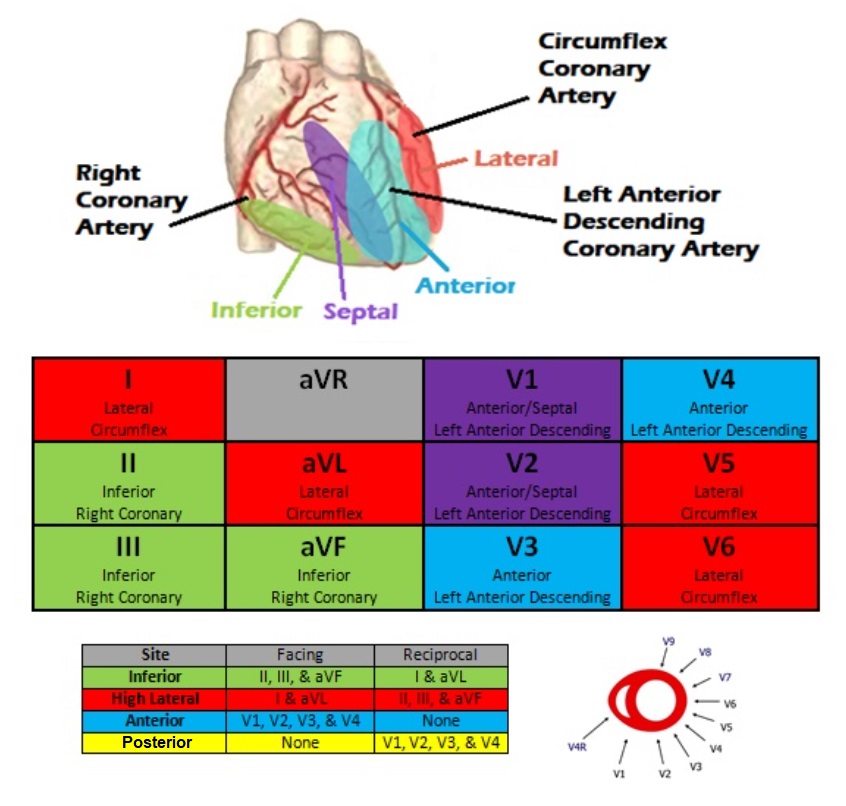
Today we are going to talk about cardiac chest pain. The heart is made of cellular tissues like any of the other organs in the body and requires a constant supply of oxygen to perform its daily functions. Cardiac ischemia is the beginning of cellular death due to lack of adequate oxygen to the tissues of the heart. Cardiac infarction is a later condition where the cardiac tissue has died. Ischemia/Infarction can sometimes be noted on a 12-lead electrocardiograph (ECG/EKG), because this dead and/or dying tissue does not allow correct electrical conduction through the heart. I say CAN, because this is not always the case. An “ST” Segment Elevation Myocardial Infarction or “STEMI” is defined as ≥1mm of elevation in two or more contiguous leads on a 12-lead ECG. Contiguous refers to portions of the heart that are located in similar locations, but we’ll talk about those in a minute.
So let’s review each part of the ECG cycle:
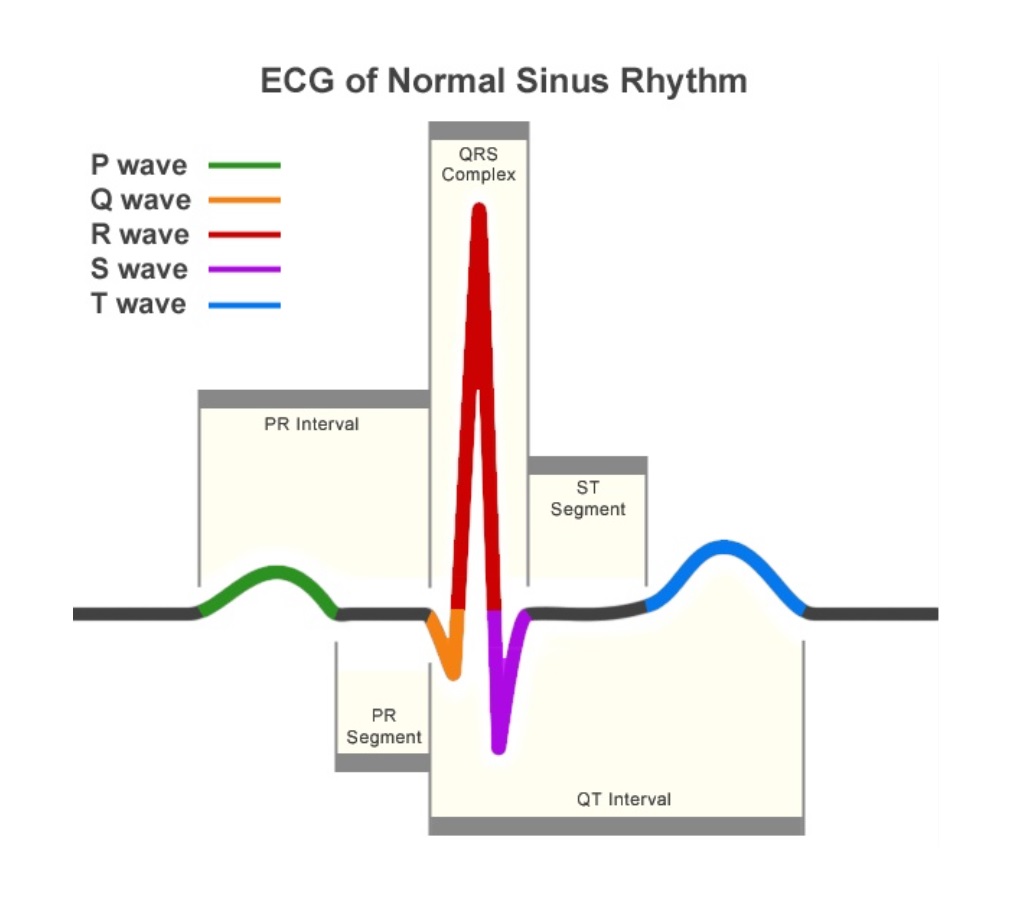
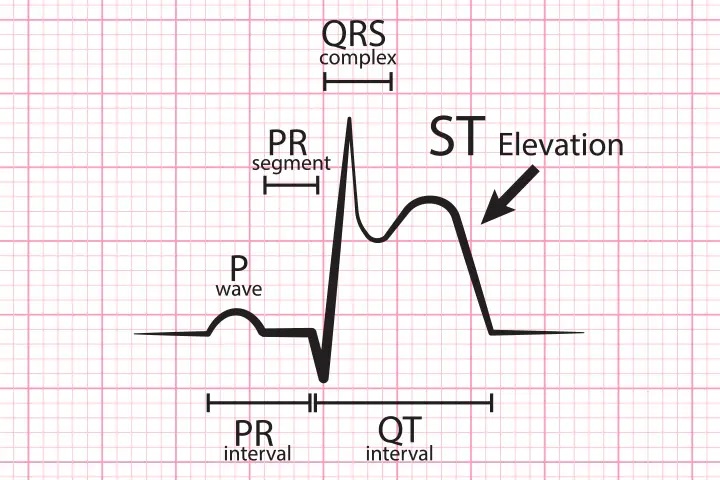
In a normal healthy patient, there should be a well-defined QRS for every beat. A patient having a myocardial infarction can have ST segment elevation, which is the ST segment is elevated above the isoelectric line, or the baseline of the ECG rhythm. If this segment is elevated above 1mm, or one small box this is classified as “ST elevation”. Now, that doesn’t automatically mean you can call this as a STEMI. Another requirement is that you have this ST elevation in two or more contiguous leads.
Contiguous leads are two or more leads that are in the same location of the heart. A 12-lead ECG can be broken down into multiple sections: Inferior, Lateral, Anterior and Septal.
If a patient doesn’t have a STEMI, that doesn’t mean that they aren’t having a heart attack, they could be having what’s referred to as a Non-ST Elevation Myocardial Infarction (NSTEMI). But if there isn’t elevation on the monitor, how can you know they are having a heart attack? Well, this is diagnosed after a positive Troponin level is noted and/or an electrocardiogram is performed. Troponin is a protein that is found in the heart. During cardiac damage, the protein is sent into the blood and can be present in lab findings.
The easiest way to think about this is to think about a motor vehicle collision on the interstate. If there has been a collision, there is bound to be fragments of the vehicles in the roadway. Eventually these fragments will be spread over a greater area as traffic slowly continues. Troponin is like these fragments of car pieces. They will spread throughout the blood stream and when labs are taken, a positive troponin level can be detected. 0-0.4ng/ml is considered a normal Troponin level; however, for the emergency setting, anything over 0.01ng/ml is possibly indicative of cardiac damage. Now most ambulances do not have capabilities to check for this protein, which is why all chest pain complaints should be treated equally until proven to not be a STEMI upon your arrival in the ED.
Most hospital systems in the United States allow their EMS agencies to “activate” the cath lab from the field. When an EMS provider notes the patient to show a STEMI on 12-lead ECG, they will notify the hospital of these findings and in turn notify the cardiac catheterization team. This team can be on site, or “on call”. This is why it is so important to activate the team as quickly as possible. If they are “on call”, they will have to drive to the facility and prepare for the procedure which could be up to an hour. The reason most services allow their EMS personnel to begin this process is to cut down on this time. The earlier they can activate this team, the better the chances the patient will have a positive outcome.
Now when it comes to medications, the American Heart Association suggests the administration of the following medications: Oxygen, Aspirin, Nitro and Morphine/Fentanyl.
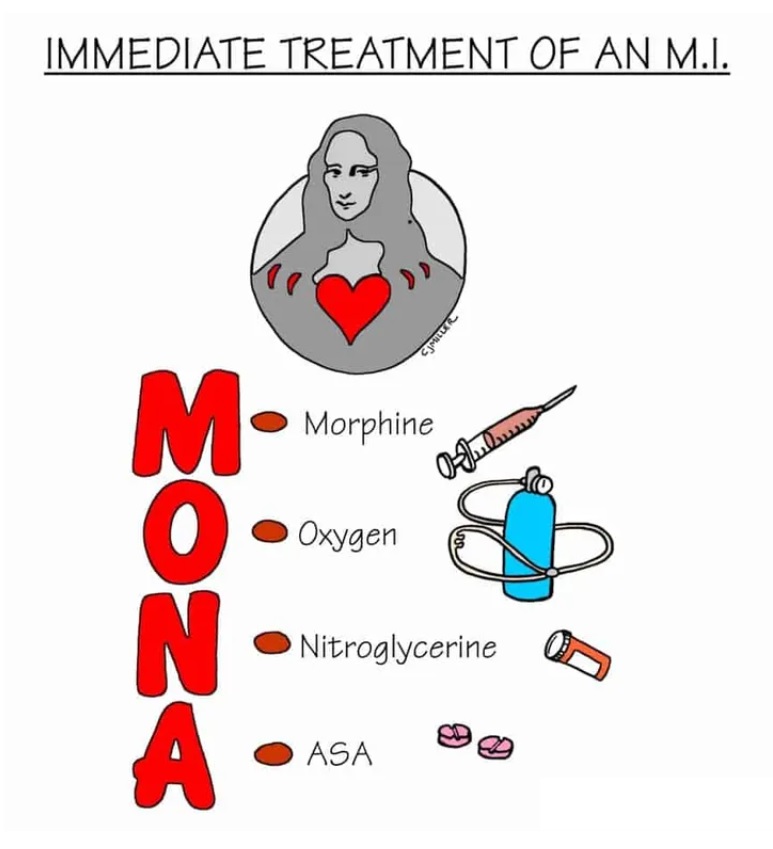
- Oxygen should be titrated to an SPO2 of 90%. In high concentrations oxygen can have vasoconstrictive properties. Now, your heart needs oxygen so you want to make sure the patient is getting what they need, but you want to make sure you don’t give “too much”. This can be administered anywhere from 2-15lpm via nasal cannula, simple mask, non-rebreather mask, or even bag-valve-mask as needed.
- Aspirin (ASA) is a platelet agitator, or inhibitor, meaning that it will not allow your platelets to clot. This gets confused with blood thinners, but it not actually a blood thinner. Aspirin is administered at 324/325mg depending on the type administered. “Baby Aspirin” is the preferred version, which is packaged in 81mg chewable tablets. Four of these pills is 324mg. If the patient is given an adult aspirin, then the dosage is 325mg of one pill. When giving adult aspirin, you want to make sure it is not the enteric coated version. This is a “time released” version. You also need to be hesitant with aspirin administration to a patient with a recent bleed, most importantly a gastro-intestinal bleed, or someone who may be allergic to “acetylsalicylic acid” which is the medical name for aspirin.
- Nitroglycerin is a vasodilator that will hopefully vasodilate all of the patient’s blood vessels to allow some blood past the clot causing the chest pain. Nitro is administered at 0.4mg sublingual (under the tongue) in pill or spray format, or via “Nitro Paste”. Nitro has sometimes been noted to decrease, if not stop, the pain associated with cardiac ischemia. Nitro needs to be given by a patient-by-patient basis. A patient who has taken any erectile dysfunction medications in the past 24-48 hours should not be given this medication. Not only male patients need to be asked if they have taken these medications because many providers will administer ED meds for all sorts of complaints. On top of that, you always want to make sure you have a patent IV in place prior to administration and the patient has a minimum blood pressure of 90 systolic. Last, but not least, you want to ensure that your patient does not have an inferior STEMI. This one isn’t an “end all be all” rule, but you need to be aware of it. If the patient is hypertensive, then administration of Nitro more than likely will not affect them. However, you need to be aware that Nitro directly effects the patient’s preload, which could “bottom out” their pressure if not administered correctly
- Morphine or Fentanyl. Most hospital systems still use Morphine for chest pain; however, many EMS systems have switched to Fentanyl. As for dosage, follow your protocol. There is a wide range of what is considered a “good” dosage for these patients. If you are worried about the medication causing any affects to the patient’s pressure or respiratory drive, then you don’t necessarily have to administer these medications. It may sound heartless, but no patient has ever died from pain alone.
At the end of the day, the best treatment you can provide to a patient experiencing chest pain is get them to definitive care as quickly as possible. Sometimes that means performing tasks on scene, but in this case it means starting a “diesel drip”.

***THIS IS A JOKE, NEVER DRIVE AN AMBULANCE ANYWHERE NEAR 200MPH!!!***