Advanced Cardiac Life Support (ACLS) is a set of guidelines established by the American Heart Association (AHA) for all healthcare workers with advanced cardiac capabilities. ACLS establishes guidelines for the following situations:
- Acute Coronary Syndromes
- Suspected Stroke
- Bradycardia
- Tachycardia
- Cardiac Arrest
- Pulseless Electrical Activity (PEA)
- Asystole
- Pulseless Ventricular Tachycardia
- Ventricular Fibrillation
Due to the length of this course, I will break this review into three parts over the next couple of weeks. This week we are going to review Respiratory Concerns, Acute Coronary Syndromes and Suspected Stroke.
First, let’s talk about respiratory concerns. As with everything else in the medical field, you want to go from BLS to ALS. If you have a patient who is breathing on their own (at an adequate rate), then obviously you don’t need to ventilate them. More than likely, a simple nasal cannula will suffice to increase their SPO2 to an adequate reading. But in the event that you do have to ventilate them, still keep this theory in mind. If you are ventilating a patient with a bag valve mask and getting adequate chest rise/fall and adequate SPO2, there isn’t necessarily a reason they need an advanced airway placed. More times than not, a good seal with the BVM mask and an oral pharyngeal airway (OPA) is all you need to maintain a patent airway.

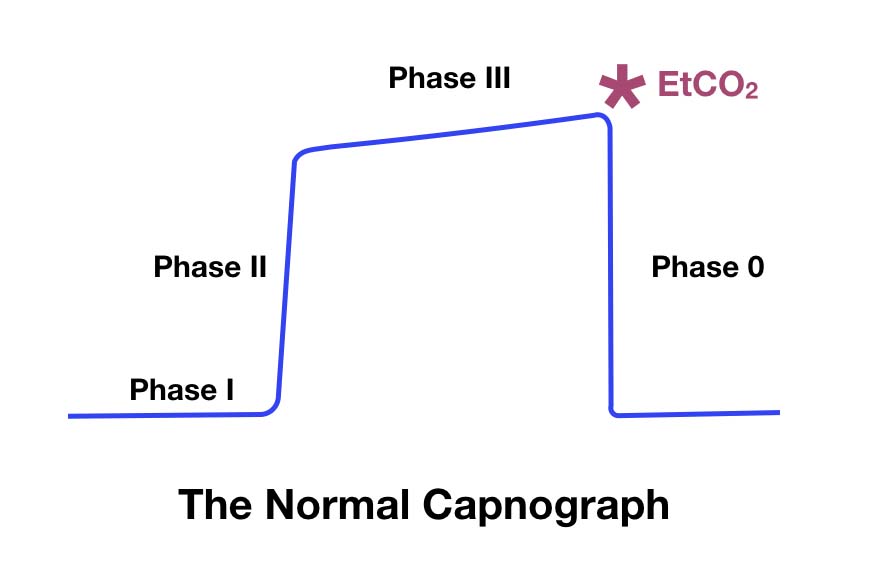
Regardless of airway placement, wavelength capnography should be monitored with any patient who is symptomatic. The general thought is that if you have an SPO2 reading than you don’t need an end-tidal capnography reading. This couldn’t be farther from the truth. These two measurements are COMPLETELY different. SPO2 measures the amount of oxygen that is coming into the body and being absorbed into the blood stream and attaching to hemoglobin. In no way does it tell you how the body is processing that oxygen. Whereas capnography reads the amount of carbon dioxide being expelled during a respiratory phase. This number indicates how the body is using that oxygen and its efficiency. Both numbers are very valuable and “paint” completely different pictures on your patient’s condition.
A couple things to keep in mind in regards to wavelength capnography during a cardiac arrest are:
- <12.5mmHg = Inadequate Compressions
- <35mmHg = Hypoventilation
- >45mmHg = Hyperventilation
Now let’s break each of these cardiac guidelines down!
But first, I would like to give the disclaimer that this information was taken from the 2020 AHA Guidelines. This information presented in this blog are guidelines and do not supersede your services policies/procedures, medical direction, and/or scope of practice.
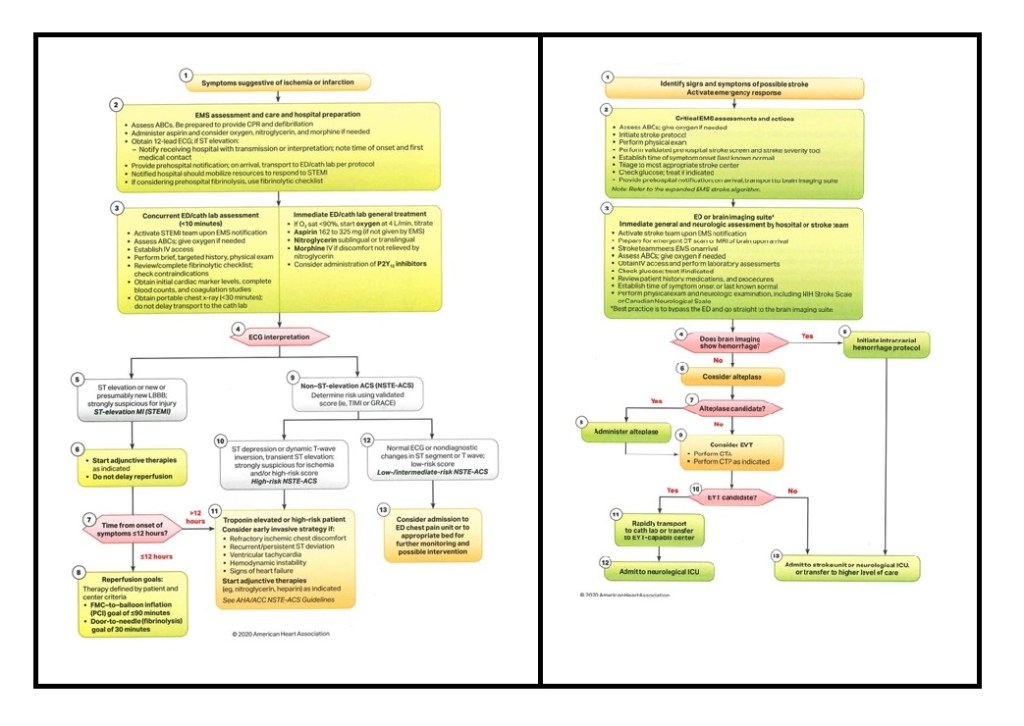
Acute Coronary Syndrome
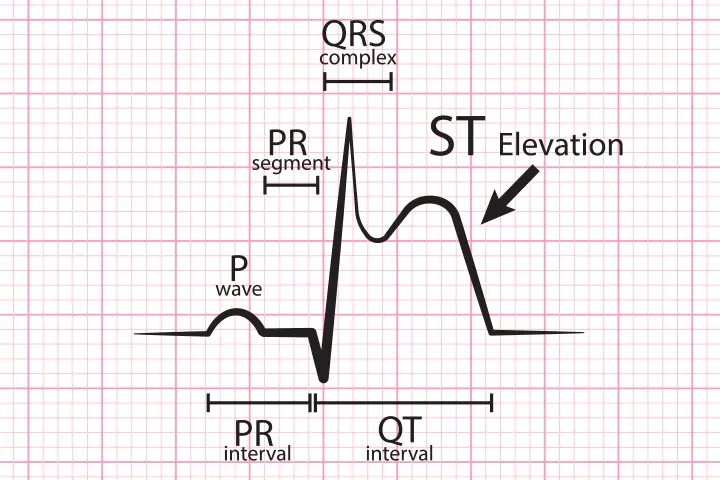
Defined as suspected cardiac ischemia and/or infarction. ST-Elevation Myocardial Infarction (STEMI) or a Non-ST Elevation Myocardial Infarction (NSTEMI) is commonly referred to as a “heart attack.” These patients need immediate intervention to halt cardiac death. We are all taught “time is brain” for strokes, but the same concept applies for the heart; therefore, early activation of the cath lab is paramount. A STEMI is currently defined as ≥1mm of ST elevation of two or more contiguous leads on a 12-lead ECG. What this means is, there needs to be more than one box of elevation in two “views” of the 12-lead ECG that correspond to one another (Inferior, Septal, Anterior, and/or Lateral). Now, on an NSTEMI you won’t see ST elevation, hence the “NON-STEMI”, so for these patients the only indication that cardiac cellular death is occurring is an elevated Troponin. Troponin is a protein that is present during cardiac ischemia. A “positive” troponin is any level above 0.01ng/ml. If either of these findings are noted, the cath lab should be notified immediately and treatment should begin as soon as possible. Definitive treatment for this type of patient is to get immediate reperfusion of the muscle tissue, via thrombolytic administration and/or thrombectomy. The “Door to Needle” goal for these patients to receive fibrinolysis is <30min, and a “First Medical Contact to Balloon” goal of ≤90min. These patients should be treated with:
- Oxygen (as needed)
- Aspirin – can be instructed to be given by the 911 Emergency Medical Dispatcher (EMD)
- Nitroglycerin
- Morphine/Fentanyl (as needed)
Patients should receive these medications in this order; however, the acronym “MONA” or “FONA” is commonly used to remember the chest pain medications.
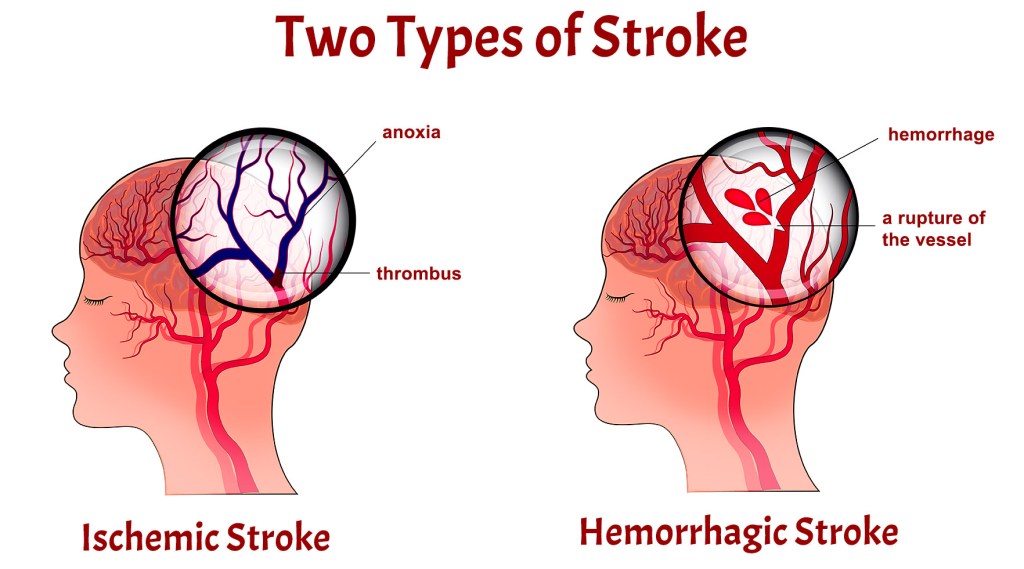
Suspected Stroke
Defined as when a patient presents with unilateral symptoms, including but not limited to:
- Facial Droop
- Slurred Speech
- Arm Drift
- Severe Headache
- Sudden Onset of Confusion
- Numbness/Tingling
As I said before, “time is brain” for these patients so again, early activation of the neurology team is paramount. The more time that goes by the more damage that is going to be done to the brain tissue, which may be irreversible and sometimes fatal. In the event that your patient is experiencing stroke-like symptoms, the patient requires immediate attention by either a Primary or Comprehensive Stroke Center. The onset of symptoms is one of the most important parts of stroke care, mainly because of Tissue Plasminogen Activator (tPA). tPA is typically administered within the first four hours of the onset of symptoms. Prior to tPA administration; however, a non-contrast CT scan will be needed to rule out a hemorrhagic stroke. This scan should be performed within 20 minutes of arrival in the ED and should be read within 45mins. Both of these interventions can be performed by a “Primary Stroke Center.” In the event that your patient needs further evaluation, the patient will need transport to a “Comprehensive Stroke Center” for thrombectomy. Lastly, the administration of oxygen should be titrated to 94% for these patients. At high volume, oxygen has vasoconstrictive properties; therefore, we don’t want the vessels to constrict any more that necessary for these patients.
With stroke patients, it is very important to not only document the onset of symptoms, but also to note any blood thinner administration in the last 24 hours. This can be hard to determine if a patient is unable to speak and there are no bystanders/family/friends present.