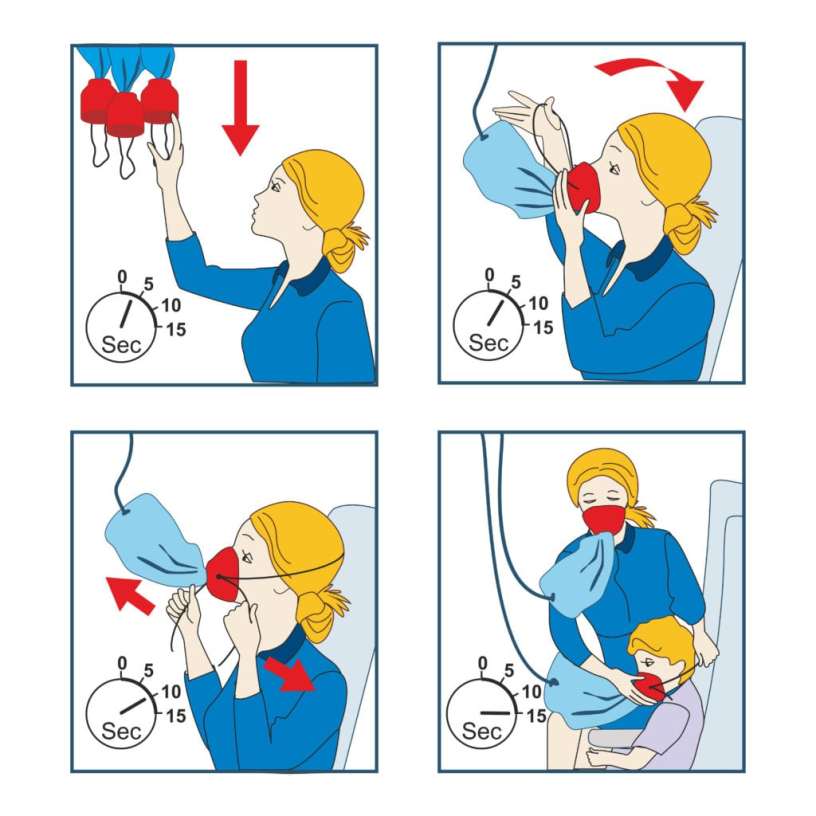
If you’ve ever been on an aircraft and actually listened to the safety information at the beginning of the flight, you’ll know that in the event of an emergency, oxygen masks will be deployed from the ceiling and you are supposed to apply your own mask before helping others. But why is that? If you have a child with you, wouldn’t it be smarter to put his or her mask on first???

Well, this all boils down to that you can’t help others if you don’t help yourself first. In the event of a plane crash, you need to insure your own safety so you can assist others in need. If this scenario was flipped, you would help the child get his or her mask on; however, you could possibly parish and then fail to render further aid to the child who needs you.
So why go on this tangent you may be asking? Well, this directly relates to all of us in public safety. This includes mental health as well as your overall health. These two topics are SEVERELY lacking in this field and I myself am guilty.
We eat like crap, don’t work out and have severe risk factors for every mental health condition under the sun. So why do we, who are trained to help others in need, refuse to take care of ourselves?
Speaking from personal experience, it’s partly because we are lazy. I for one don’t mind eating healthy food (with the occasional “treat” here and there), but I can’t stand preparing food. We work 12, 14, and 24 hour shifts (when we don’t get a late call…), and the last thing we want to do is come home and have to prepare things for the following day. When I get off shift, I’m emotional and physically drained. I barely make it through the drive home and then into the shower, before passing out in bed. So, just for convenience, it makes sense. But in the long run, we are doing our body’s more harm than good.

It’s much easier to leave everything until the next morning and then just grabbing some fast food in between calls, but yet again, that’s doing more harm than good.
The next issue is an active lifestyle and exercise, or lack of them, to be more accurate. This again is thanks to laziness. I can only speak from personal experience, but the last thing I want to do after working 2-3 12 hour shifts is to work out. I know that it’s good for me and that I should be doing it, but like 90%, if not more, of the American population, I’m lazy. This is directly affecting my overall health and in some ways, harming my patients by potentially not having the strength/agility that I should have to care for others. This became APPARENTLY clear a couple years ago when I had a patient who fell on a walking trail on a nearby mountain. The patient was approximately two miles up the mountain over VERY rough terrain. I was about a mile in and I wasn’t sure I was going to be able to make it to the patient, let alone care for them and then remove them from the trail. Luckily on this call, the fire department had an all-terrain vehicle that was able to pick us up and get us to the patient a little faster. This should have been a wakeup call for me, but it wasn’t until I hurt my back that I decided a life change needed to be made. But it shouldn’t have taken me that long to realize there was an issue that needed to be addressed.

Finally, we have the issue of mental health. In recent years we have made leaps and bounds in this aspect of our jobs, but it is still nowhere near where it should be. Until agencies start respecting high stress call response as an emergency in itself, then we will never get to where we need to be. I for one had a supervisor in the past who would rush us back into service after every call, no matter what the previous call was, just because “calls were holding.” I understand that we have a duty to act and can’t leave emergency calls without EMS response, but that goes both ways. Since the COVID pandemic, we have seen a MASSIVE drop in staffing. This is in part to pay concerns, vaccine mandates, and multiple other reasons, but the big problem is the amount of burnout in this field of work. No matter the type of call, we all respond in our own ways. Like everything else in this world, you can’t put a blanket rule over the entire profession. What one person blows off as “just another call,” may be MASSIVELY detrimental to another. Here’s an example: before my daughter was born I cared for kids, but I was never really emotionally invested. I did what I needed to do in regards to patient care, but that was it. Since having my daughter, I am a completely different patient provider. Child abuse is a prime example of what I’m talking about. It used to upset me that someone could do that to a child, but now it INFURIATES me and it’s almost as if its personnel now. So obviously I am going to take a cardiac arrest of a child worse now than I did before I had my own child. But that one’s a “no brainer”. How about a simple fender bender where someone’s car is still drivable. Most of us would just blow this off as any other call, but what about the crew member who was JUST in his or her own accident the day before? What appears to be a “simple call” could trigger a MASSIVE post-traumatic stress response for the right crew member.

I say all of this in the hopes that we as a profession wake up to some of the most important aspects of our profession, our own health. Like I said at the beginning of this blog, you can’t help others until you help yourself. I am actively making massive changes in my lifestyle to do exactly that, and I invite anyone who is interested in joining me. With just a few minor changes, we can greatly improve this career field for ourselves, our coworkers, and our patients.