One of the most daunting parts of becoming a Paramedic is learning all of the different rhythms and abnormalities. There are entire books upon books written on the subject. But what about ECG’s for EMT’s? Some programs go over the basics of ECG interpretation in EMT school, however it is not a requirement of the course curriculum.
So does that mean that EMT’s don’t need to know about ECGs???
While the task will ultimately fall on the Paramedic, there is no harm in an EMT knowing the basics of ECG interpretation and the importance of lead placement. Yes that’s right, I said lead placement. I know placement seems to be just yet another thing that is stressed in school, but goes to the waste side out in the field, but that’s not the case in this scenario. To explain this we need to talk about how an ECG is taken.
I want you to visualize a teddy bear. Now, with your camera take a right sided profile picture of the bear, like this:

Now if you were to take the picture from too high up (and not right next to the bear), you would get a different picture right? Well this view on an ECG gives you Lead I. Now if you were to put the bear/balloon on the ground and take this same picture standing up (looking downward slightly), you would have Lead II. So that slight change of camera placement gives you an entirely different view of the heart. Now this example is very large, so imagine you are trying to take a picture of something the size of your fist. So you can see that even a milimeter of change can COMPLETELY alter the view in the picture you are taking, and that’s what happens when placement of the electrodes is done incorrectly. So what may seem to be redundent and pointless, is actually VERY important.
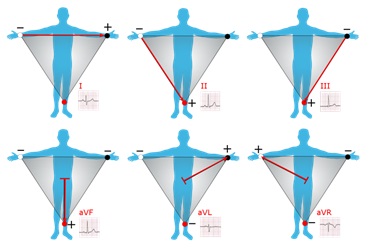
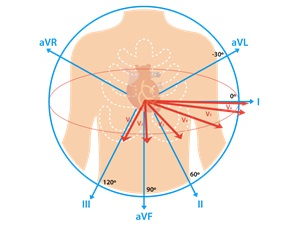
Now that’s just the limb leads (I, II, III, aVR, aVL, & AVF), but what about 12 leads?
The limb leads are all taken on the same plane of the body, as if it were a flat object. But what about from front to back and vise versa? That’s where the 12 lead electrodes come into play. They are arranged to take multiple views of the heart across the chest. This is important to locate any abnormalities of the heart, most importantly a myocardial infarction or “heart attack”. Im not going to dig too deep into their views, but knowing their correct placement is of the upmost importance.
So now that we know about lead placement, let’s talk about the basics of ECG interpretation. Each part of the ECG wave tells a “different story” per say. Each chunk of the wave has a name and shows part of the cardiac beat.
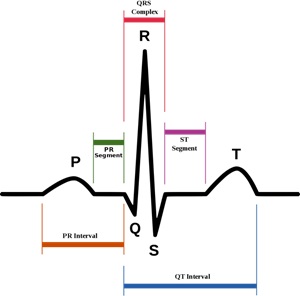
Now each “segment” has a meaning and a measurement it needs to be within, but we aren’t going to get into all of that today. Let’s just talk about the single letters you see here and their meaning.
Remember “Flub-Dub”??? That’s what you’re seeing here.
The “P” Wave shows the electrical discharge of the atriums of the heart (the top), so the “flub”. The “QRS” is the electrical discharge of the ventricles of the heart (the bottom) as well as the electrical recharging of the atriums (top), this is the “Dub”. And finally the “T” wave represents the electrical recharging of the ventricles (bottom), but this part is silent. So why is the P wave so little compared to the QRS? Because the top chambers of the heart only need to pump blood into the lower sections of the heart, where as the bottom chambers of the heart need to pump blood to the lungs and to the rest of the body. The more work required, the more electrical input required as well. Think of this like the difference between a small car and a semi truck. The little car is NO WHERE near as loud as the truck right?
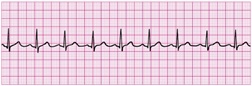
Each of these “P”, “QRS”, & “T” waves represent one beat of the heart, so “flub-dub”. Now when you put multiple of these complexes together you get an ECG rhythm. Remember how I said there are measurements of each of these intervals? When reading an ECG, you need to decipher what rhythm you are seeing, according to a list of rules for each rhythm. Now, we aren’t going to get into each of these different rhythms today, but let’s talk about the most important ones.
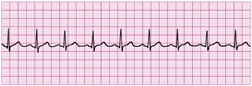
This is referred to as “Normal Sinus Rhythm”, which is the normal heart rhythm with a matching pulse noted. Now this name changes depending if it’s too fast (Sinus Tachycardia) or too slow (Sinus Bradycardia) and everything in between. All of the waves are present and everything is within a normal range. This is a good day.
But what about a bad day? Here are those “bad days” aka Lethal Rhythms.
First off, let’s talk about the “shockable rhythms”, so the ones that you defibrillate. With a cardiac monitor, the Paramedic must decide the rhythm the patient is in and act accordingly. With an AED, the machine is determining this for you. If the patient is in either of these two rhythms, the AED will give the “shock advised” notification:

Ventricular Tachycardia

Ventricular Fibrillation
But what if the patient does not have a pulse and the AED states “no shock advised”? That is because the patient is in one of these two rhythms:
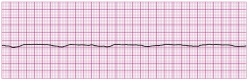
Asystole or “Flat Line”
Easy enough right? What about this???
Wait a second, isn’t this the same rhythm I said was NORMAL?!?!? Yes, I did, but I also said that patient has a pulse. This patient has this rhythm without a pulse, which is called:
Pulseless Electrical Activity or “PEA”
That means that the heart is still charging and discharging electrical current, however the muscle tissue isn’t moving.
In these two rhythms, the patient should be given continuous CPR and assisted respirations along with any other treatments deemed necessary by your service’s protocols.
This was a VERY brief overview of ECGs, but is the down and dirty basics that I feel like every responder should know. If you’d like to learn more, I would highly recommend taking an ECG class to learn up on ECG interpretation. This may be an ALS skill, however it can never hurt to have an extra set of trained eyes on the issue. At the end of the day, we are all on the same team and here to help those who may need us. So what harm is there for having a little extra knowledge!